You're Not “Too Young” For Hormones to Matter
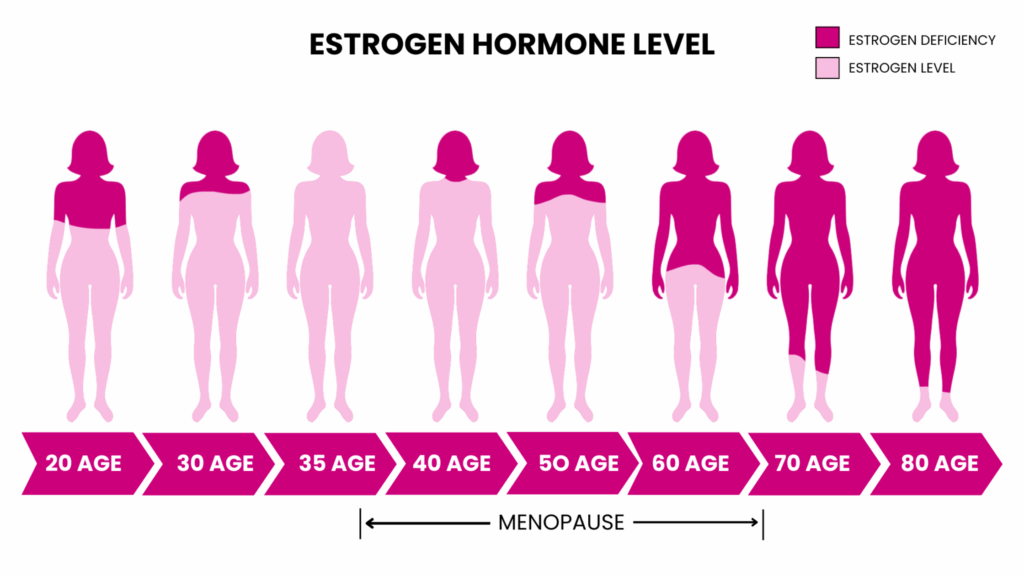
If you are over 35, there is a very real chance your hormones have already started to shift… and no one told you.
That's not your fault. Most doctors get very little formal training in menopause or perimenopause. One survey found fewer than one in five OB-GYN residents received formal menopause education, and only about 7% felt prepared to treat it. The Hub
So women walk into appointments describing very real symptoms and walk out with “you’re just stressed” or “welcome to aging.”
Let’s fix that.
Table of Contents
ToggleWhat Perimenopause Actually Is
Menopause is one day. It is the day you hit 12 months without a period.
Perimenopause is the long, messy runway leading up to that day. For many women, symptoms begin 7 to 10 years before menopause. Rutland Regional Medical Center
That means a woman in her late 30s or early 40s can absolutely be dealing with hormone related changes… even if her cycle looks “mostly normal” on paper.
Early Hormone Warning Signs Most Women Miss
Hot flashes and night sweats get all the press. Up to 80% of women have vasomotor symptoms at some point in the menopause transition. The Menopause Society
But the earlier, quieter warning signs often get brushed off as “just life”:
- Weird, inconsistent periods
- Waking up at 2 or 3 a.m. for no good reason
- Sudden anxiety, irritability or “I don’t feel like myself”
- Feeling thicker through the middle even when your habits have not changed
- Leaking a little urine when you sneeze, laugh or jump
- Brain fog, word-finding issues, or feeling mentally “slower”
- New joint pain, headaches or migraines
- Itchy ears, dry eyes, drier skin and hair
- Lower libido or discomfort with sex
On their own, each symptom feels random. Together, they paint a hormone picture.
Why This is About More Than Comfort
Estrogen, progesterone and testosterone are not just “period hormones.” They impact your brain, bones, muscles, heart, sleep, metabolism, mood and more.
When those hormones decline, your body does what it can to protect you. One way is by storing more visceral fat around your organs. That fat is metabolically active and drives inflammation and insulin resistance, which helps explain why about four in ten U.S. adults are now living with obesity, with the highest rates in midlife. CDC
So this is not just about hot flashes. It is about long-term health and longevity.
The Science is Changing… Your Doctor May Not be Caught Up
For years, hormone replacement therapy (HRT) was labeled as “too risky” because of early interpretations of the Women’s Health Initiative (WHI). Newer analyses make it clear that the original message was oversimplified. Estrogen therapy in appropriately selected women can lower breast cancer incidence and mortality and reduce overall health risks, especially when started earlier in the menopause transition.
The problem is many clinicians are still practicing from the original headlines, not the updated data.
That is why you can absolutely love your doctor and still not be getting the best hormone guidance. I trust Midi Health. I use them, love them, and they take most insurance and it's from your own home!
What to Actually do Next
You do not have to become a hormone expert, but you do need to become the expert on you.
Here is where to start:
Track your symptoms
Use the notes app on your phone. Jot down:
- Date
- Where you are in your cycle (if you still have one)
- What you felt: sleep, mood, bleeding, pain, brain fog, weird “one-off” things
Patterns make it much easier for a good clinician to help you. Look for someone who:
- Specializes in midlife women’s hormone health
- Uses both symptoms and lab work
- Is familiar with up-to-date menopause guidelines, not just the original WHI headlines
You are interviewing them as much as they are treating you. It is OK to ask about their training and their approach to HRT and non-hormonal options.
Understand your options, not just “yes or no” to HRT
For some women, bioidentical hormones are life-changing. For others, medical history or personal preference means they start with:
- Strength training
- Better sleep timing
- Nutrition that supports blood sugar and gut health
- Stress reduction and nervous system work
- Non-hormonal medications or targeted supplements (magnesium is legit a common missing link)
The point is not “one magic fix.” It is building a plan that fits your body and your risk profile.
Start earlier, not later if you can
Emerging research suggests that starting hormone therapy closer to the onset of menopause can ease the transition and may reduce risks like cardiovascular disease and all-cause mortality in the right candidates.
If you are already postmenopausal, it is still not “too late” to ask what is appropriate for your age and history.
You're are not broken; you're a woman in a hormone transition that our medical system has largely failed to prepare you for.
The more you understand perimenopause symptoms and early hormone warning signs, the easier it is to advocate for yourself, find the right clinician and put together a plan that lets you actually feel like you again.
Love you, mean it,
Chalene
P.S. Sometimes I drop an affiliate link for you. If you use it, I may get a kickback, but you often get a discount too. I only recommend things I trust, have studied and genuinely love. xo